As part of the Office of the Assistant Secretary for Technology Policy’s (ASTP) vision of “better health enabled by data,” we are committed to advancing health equity and person-centered ways to promote the interoperable exchange of data on patients’ health-related social needs (HRSN) and broader social determinants and dynamic social drivers of health (SDOH). In support of this effort, ASTP conducted several studies in the past year to better understand whether routine screening combined with capturing data in a structured format could facilitate immediate and downstream use of data collected through such screening as well as how the availability of dedicated resources or strategic partnerships with community organizations impacts providers’ ability to address patients’ HRSN.
Our measurement approach
To advance health equity data interoperability, our measurement efforts at ASTP track whether providers are screening and how screening is conducted including the types of data captured, frequency of screening, and methods by which data are collected. This enables a broad view of screening activities to better understand how easily information can be shared and effectively used for different purposes. While HRSN and SDOH data are often used by providers to inform discharge planning and clinical decision-making, data captured in a structured or standardized format in electronic health records (EHRs) can help facilitate the exchange and use of data for a range of purposes involving exchange or coordination with other organizations. This includes, for example, making referrals to social service organizations and other types of downstream uses, such as informing community needs assessments and population health analytics.
Measuring screening approaches and implications for use
Types of screening and support for addressing SDOH and HRSN
An ASTP study published July 2024 in Health Services Research identified notable variation in the types of information collected by hospitals—consistent with prior work—as well as in the availability of dedicated programs, strategies, or partnerships to address HRSN. We found that hospitals with a program or strategy to address HRSN and SDOH had significantly higher rates of screening and usage of data for various purposes including to make referrals to social services, conduct population health analytics, and help assess community needs.
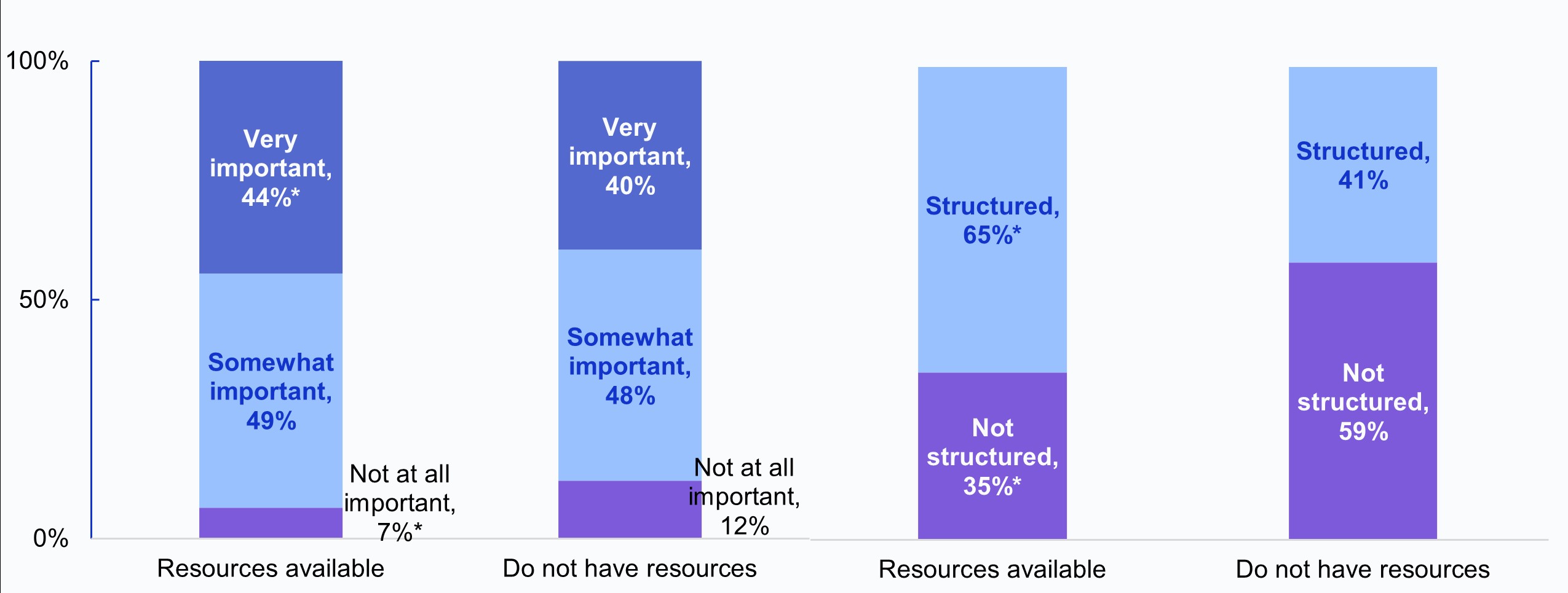
In a recent ASTP data brief examining trends in the documentation of SDOH and HRSN by family medicine physicians, we identified a similar linkage between the availability of resources and screening for HRSN. In 2022-2023, physicians who believed their clinic had resources available to address social needs placed greater importance on having access to SDOH data and had higher rates of structured HRSN documentation, indicating a relationship between how data are captured and whether those data can be used to improve patient and population health.
Family physicians’ rated importance of having access to external SDOH data (Left) and use of structured methods to document HRSN (Right), by availability of resources and tools to address patients’ social needs.
Source: ASTP Data Brief No. 75
Consistent with these findings, in a recent ASTP-supported qualitative study published in the Journal of the American Medical Association (JAMA) Network Open, an examination of clinicians’ experiences with screening and documentation of SDOH data revealed that clinicians with limited resources to address social needs did not feel comfortable screening and documenting these data.
Routine screening
In an ASTP study published in the Journal of the American Medical Informatics Association (JAMIA), routine social needs data collection among hospitals was associated with a greater likelihood of using the information collected for various purposes. Encouragingly, routine screening is on the rise; 61% of hospitals engaged in routine screening in 2023, up from 54% in 2022. While there has not been comparable measurement of routine screening among office-based physicians, the broader shift towards value-based care and increased attention to incorporating screening for SDOH and HRSN as part of standard practice, particularly for family medicine practices, suggests the promotion of routine screening among physicians is part of a larger effort to make HRSN and SDOH data available for use at the point of care.
Structured data collection
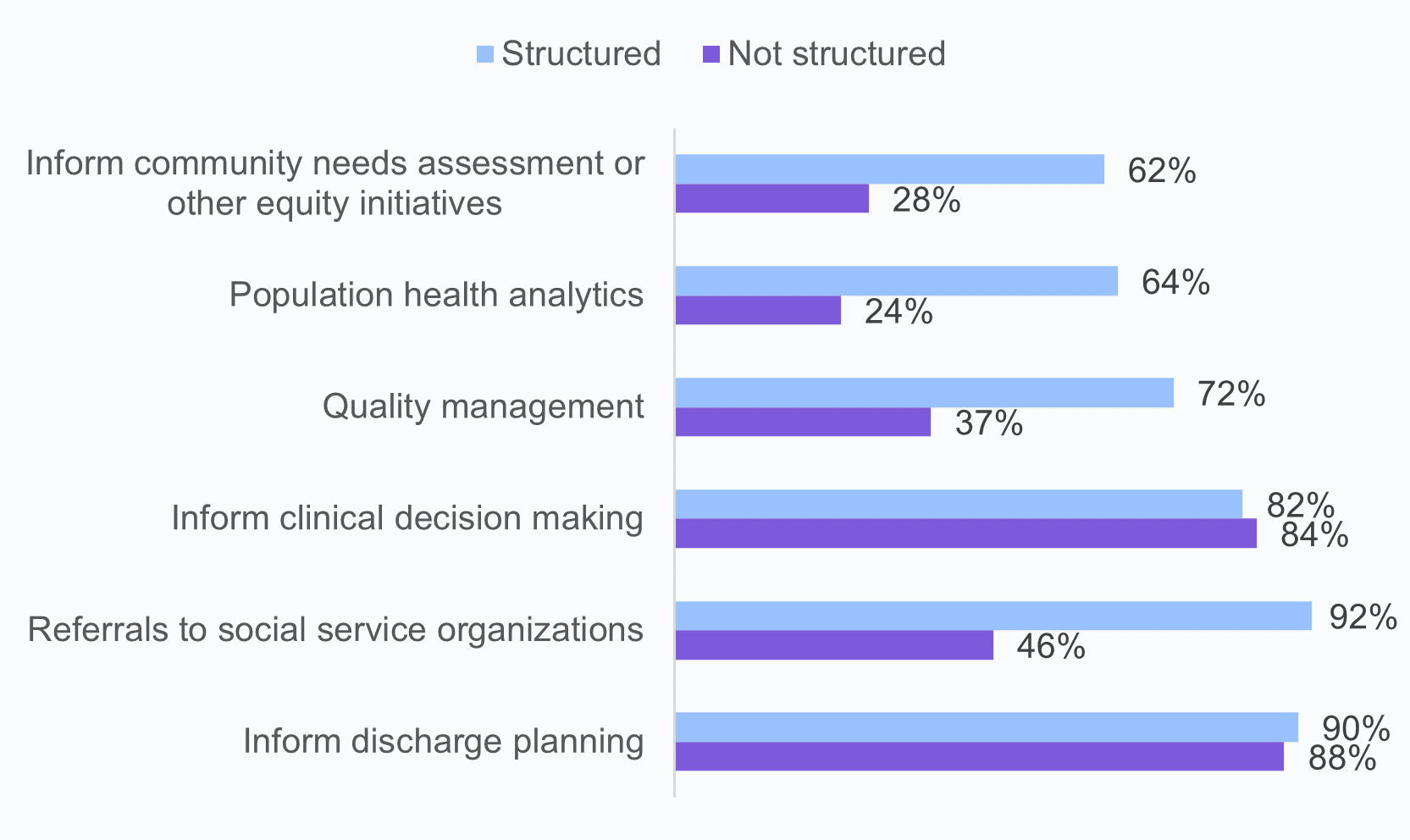
In a recent study co-authored by ASTP and published in the Journal of General Internal Medicine, we used data from two surveys of physicians to look at the different methods physicians use to document SDOH and HRSN in their EHR and how this relates to use.
While nearly three-quarters of hospitals (72%) in 2023 collected HRSN data in a structured format using an electronic structured screening tool (i.e., by checking a box or button in the EHR) or by entering it as a diagnosis (i.e., ICD-10-CM Z codes), only one-third of office-based physicians (33%) and 56% of family medicine physicians reported using structured methods in 2022.
Implications for Use
Hospitals that collected HRSN data in a structured format had significantly higher rates of using data captured through screening for downstream uses such as population health analytics, and for purposes involving coordination or exchange of information with other organizations, such as making referrals for social services. Similarly, physicians who documented HRSN data in a structured format had higher rates of using data for making referrals compared to respondents using free-text notes.
Relationship between the methods hospitals use to collect social needs data and different uses of data collected through screening, 2023.
Source: Authors’ analysis of American Hospital Association Information Technology Supplement data. Data originally published in: Role of routine and structured social needs data collection in improving care in US hospitals | Journal of the American Medical Informatics Association | Oxford Academic
Together, these findings suggest routine data collection in a structured format that enables consistent capture of data elements may help facilitate the use of SDOH and HRSN data for a broad array of uses. We also found that a lack of resources may impede the ability of hospitals and physicians to effectively use data captured through screening. This speaks to the importance of continuing to advance efforts to establish and strengthen partnerships with community and social organizations to ensure that information shared can be used to coordinate care and improve patient and population health.
Looking Forward
ASTP envisions a future in which health equity data—including data on patients’ HRSN and community SDOH—is not only interoperable but can be harnessed by healthcare and social service organizations to deliver high quality care and address root causes of health inequities. In 2023, as part of the HHS Data Strategy, ASTP (then ONC) was formally designated as the HHS lead for the development and harmonization of interoperability standards between health and human services. In collaboration with our government and industry partners, ASTP will continue to work to advance SDOH and HRSN data interoperability. The collection of data using consensus-based standards—such as those developed through the Gravity Project to represent SDOH data elements—will help ensure that data can be used to inform clinical decision-making and care planning, as well as enable the provision of social needs services and support downstream use. However, data are most actionable if providers have relationships with community partners or resources available to address identified needs, which in turn can help build patient trust that sharing social needs data with providers will help meet their needs.
It will be important to continue to study providers’ use of data captured through screening as well as the capacity of the community to participate in equitable, electronically enabled screening and referral practices. Together, efforts to increase consistent data collection and those aimed at building a more integrated health and social care system are critical to ensuring that screening initiatives can create real value for patients, providers, and their communities.
RESOURCES:
With CMS’ introduction of new screening requirements for eligible hospitals participating in the Inpatient Quality Reporting Program add incentives for Merit-based Incentive Payment System eligible clinicians, identification of patients’ HRSN is becoming widespread with 83% of non-federal acute care hospitals and 63% of office-based physicians (including 72% of family medicine physicians) screening for patients’ HRSN as of 2022.